Key Takeaways
- Autism (ASD) and Attention-Deficit Hyperactivity Disorder (ADHD) are both neurodevelopmental conditions with overlapping and opposing characteristics.
- "AuDHD" refers to the co-occurrence of autism and ADHD, affecting an estimated 50% to 70% of autistic people.
- Characteristics like social-communication differences, routines, and sensory experiences can appear in both conditions.
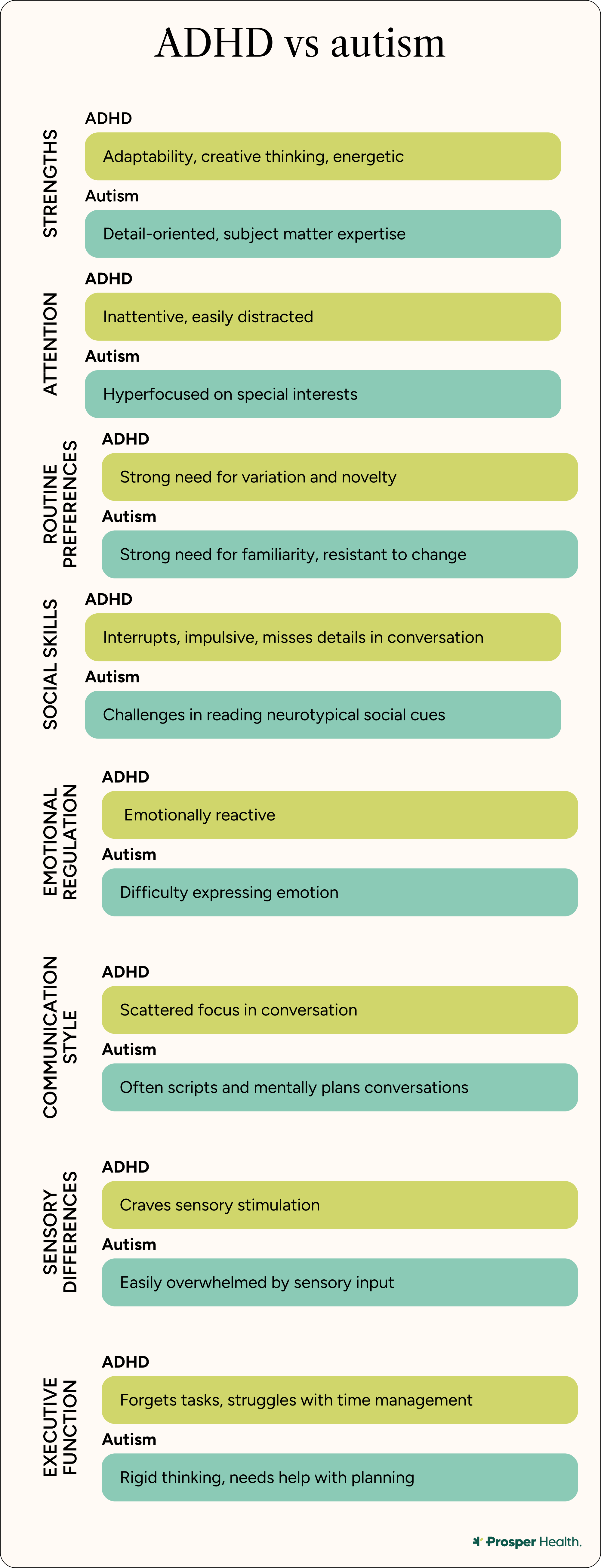
- Attention differences are a key distinguishing factor. Inattention, impulsivity, and hyperactivity are core diagnostic criteria for ADHD and less so for autism.
- Diagnosis for both conditions involves clinical assessment and specific DSM-5 criteria, and neurodiversity-affirming care is crucial for treatment and support.
There is not a day that goes by that I don’t ask the question, “Is it ADHD or autism?”
As the parent of an AuDHD child—AuDHD being a colloquial term used to describe the dual diagnosis of both autism and ADHD—I still have difficulty differentiating between the two diagnoses. Is her stimming an autism or an ADHD trait? Which of her Individualized Education Plan (IEP) accommodations at school are tailored to her autism, and which ones are tailored to her ADHD? How is her ADHD medication affecting her autism traits?
My experience is with my 9-year-old daughter, but this dilemma is equally accurate for many adults. If you’re neurodivergent in any capacity, you’ve likely had moments where you’re comparing your characteristics, trying to determine if they could be a sign of autism, ADHD, or both.
AuDHD is becoming increasingly common among neurodivergent people, and those with both diagnoses deserve a clear understanding of autism and ADHD, and what it means when they co-occur.
That said, the two conditions are not the same! Many people will only get diagnosed with one condition or the other, so it's essential to understand how they differ.
What is Autism?
Autism, or autism spectrum disorder (ASD), is a developmental disorder that affects how someone’s brain works. These brain differences can cause someone to socialize and/or behave in unique ways considered outside allistic (non-autistic) or neurotypical norms.
According to the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5), there are two main symptom or characteristic areas of ASD:
- Deficits in social communication and interaction
- Restricted, repetitive behaviors (such as stimming), interests, or activities
Some potential characteristics of ASD include, but are not limited to:
- Differences in eye contact
- Differences in body language
- Strong preference for routine and predictability
- Repeating gestures or sounds
- Closely focused interests
- Fewer facial expressions
- Decreased awareness of temperature extremes
Although someone may present with some or all of the above characteristics, this does not automatically mean they have autism. Age of onset in childhood and its impacts on important areas of functioning are also required. ASD can only be diagnosed by a qualified clinical professional.
Those who have received an ASD diagnosis are considered neurodivergent. While it’s common for some people to use the words neurodivergent and autism interchangeably, there is a difference between “neurodivergent” and “autism.” “Neurodivergent” is a non-medical term referring to anyone living with a neurodevelopmental condition like autism and ADHD. Autism, or ASD, is the name of an official diagnosis.
While not every adult who is autistic also has ADHD, ADHD is the most common co-occurring condition that autistic people experience, according to the Cleveland Clinic. An estimated 50% to 70% of autistic people also have ADHD.
Note: In the context of autism, what might often be referred to as a “symptom” is more accurately referred to as a “trait" or “characteristic” and we’ll be using that terminology as often as possible throughout this article.
What is ADHD?
ADHD, or attention deficit hyperactivity disorder, is a condition affecting how your brain works (as is autism). Characteristics include fidgeting, difficulty concentrating, and a tendency to misplace things. However, it’s important to remember that if you have ADHD, it doesn’t mean you can’t pay attention — it’s just that much harder to focus your attention and complete certain tasks. At the same time, some people with ADHD can hyperfocus on specific goals and tasks.
An estimated 6% of adults have an ADHD diagnosis, with about half of those adults receiving their diagnosis in adulthood. Some common traits of ADHD include, but are not limited to:
- Difficulty sustaining one’s attention
- Difficulty completing lengthy tasks unless they’re considered interesting
- Difficulty staying organized
- Difficulty controlling one’s impulsive behavior and emotional eruptions
- Hyperactivity, such as feeling internally restless and fidgety
ADHD is classified into three variations:
Inattentive ADHD
This type of ADHD means you have difficulty concentrating, staying organized, and focusing on tasks. For the most part, you don’t exhibit traits of hyperactivity. People with Inattentive ADHD find paying attention to details challenging, are easily distracted, find time management difficult, and may forget to do routine tasks (paying bills on time, returning phone calls, emails, texts, etc.). Studies have shown that women are more likely to be inattentive rather than hyperactive-impulsive, which could lead to delays in diagnosis.
Hyperactive-impulsive ADHD
People with this type of ADHD find it difficult to sit still and/or remain quiet. They may habitually interrupt others and act impulsively. At the same time, people diagnosed with hyperactive-impulsive ADHD may not have as much difficulty with paying attention to tasks.
Combined Presentation
This is the most common type of ADHD, where people present with both inattentive and hyperactive-impulsive traits.
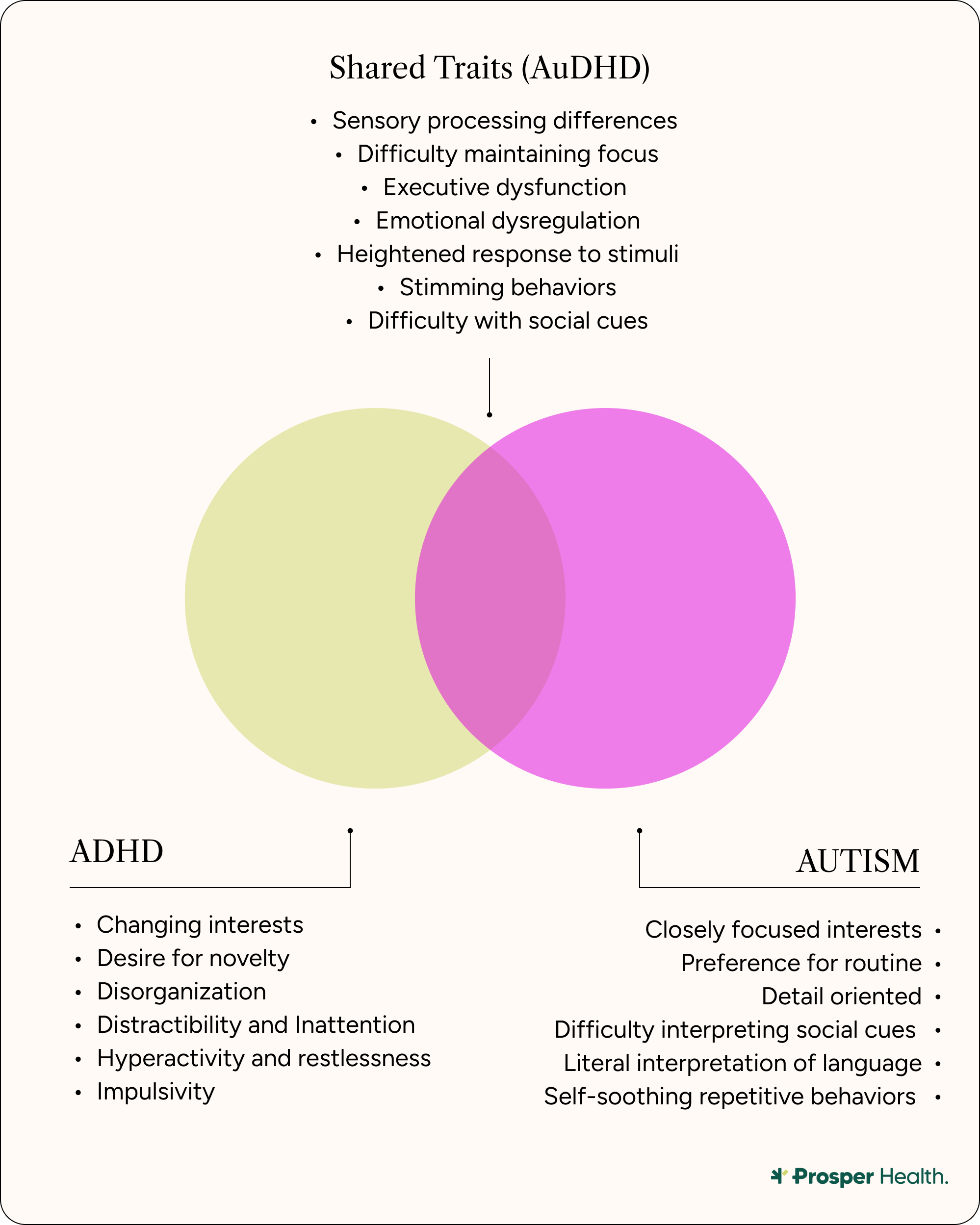
Autism vs. ADHD: What They Have in Common
The Autism ADHD overlap can be first spotted in the womb, because both are neurodevelopmental conditions. “[This] basically means they start developing early—like in utero,” says Dr. Kelly Whaling, Research Lead and Licensed Clinical Psychologist at Prosper Health.
Other examples of an Autism ADHD overlap are found in the following areas:
Social Communication
Although there is social-communication overlap between autism and ADHD, Dr. Whaling emphasizes that “the underlying reasons are often different.” For example, with autism, “it’s often because you don’t know what to do or how to interpret things,” she says.
But for those with ADHD, “you do know what to do and say, you just might be inattentive, so you miss what someone is saying and respond in a way they aren't expecting, or you're impulsive and talk over people or say things without thinking about their impact.” This kind of social behavior might look the same to outsiders, “but what's happening underneath might be totally different,” says Dr. Whaling.
Nonverbal Communication and Relationships
This is yet another example of similarities in behavior between those with autism and ADHD, even though the reasons behind the behavior can be quite different. “ADHD folks might gesticulate wildly or move around a lot, making their nonverbal communication look different,” says Dr. Whaling.
She points out how people with ADHD might miss social nonverbal cues (a common autism trait), but this is “due to impulsivity or inattention.” Also, she notes that “relationships can be hard to maintain because the social battery can be lower, similar to autism.”
Intense Interests and Sensory Differences
While intense interests and sensory differences do overlap between autism and ADHD as well, the presentation can be different.
“For autism,” explains Dr. Whaling, “the interest could be expert-level knowledge that's a core part of your identity—your life revolves around it.” For people with ADHD, however, a hyper-focused interest in something and/or a sensory processing difference “can be super intense, but fleeting.”
Psycho-social risks
“People with both ADHD and autism—most likely because of how society treats us—are more prone to depression, anxiety, peer victimization, sexual assault, and suicidal ideation or attempts,” says Dr. Whaling.
She also highlights the prevalence of emotional dysregulation in both conditions. This “can lead to self-injury, relational challenges, interpersonal conflict, etc.” It’s also common for people with autism and/or ADHD to engage in masking, or the practice of hiding one’s traits.
Key differences between autism and ADHD
Routines
Routines affect people with autism and ADHD differently, though Dr. Whaling points out that the differences can get complicated, especially if someone is AuDHD.
She explains that “autistic people absolutely require routines and sameness for regulation and predictability.” But while “people with ADHD often benefit from routine, this is really challenging because maintaining routines requires executive functioning skills that they struggle with in the first place.”
At the same time, “because ADHD is about novelty seeking and sensation seeking for a lot of people, routine can actually be extremely distressing due to boredom, and people can burn out trying to push through with a routine instead of getting their dopamine and stimulation needs met in novel ways.”
What can happen, whether you are AuDHD or have ADHD, is “this weird contradiction where you need routine but also crave novelty,” says Dr. Whaling. “Whereas autism has less of the need for unpredictability and novelty, and in fact, can often be really bothered by it (unless you have both!).”
Attention Differences
Attention differences are “probably the biggest distinguishing factor” when it comes to ADHD vs. autism in adults, says Dr. Whaling. While people with autism might have some executive functioning challenges, “it's not in the DSM as a core feature.”
For those with ADHD, however, attention differences “are the core of ADHD – that’s literally what defines it in the diagnostic criteria,” says Dr. Whaling. Impulsivity, forgetfulness, hyperactivity, inattention, etc., are not required for an autism diagnosis, but they are required for an ADHD diagnosis.
Cognitive processing
There are several cognitive processing differences between ADHD and autism. Dr. Whaling points out that research suggests “autistic people have a more literal interpretation of language, see things more concretely, and have really great pattern recognition, attention to detail, etc.” But this may not be the case for people with ADHD.
As for difficulties with executive functioning, Dr. Whaling highlights that people with autism might have challenges “shifting attention, disengaging from a special interest, and differences in joint/shared/reciprocal attention, which are quite different than the executive functioning differences of people with adhd.”
AuDHD: When Autism and ADHD Co-Occur
Prevalence
Clinicians have only been able to officially recognize the co-occurrence of autism and ADHD (AuDHD) for about 12 years: “Until the DSM-5 came out in about 2013, autism and ADHD could not be diagnosed together,” explains Dr. Whaling.
Even though the literature estimates 50% to 70% of autistic people also have ADHD, Dr. Whaling mentions the possibility that pinpointing the prevalence of AuDHD is still a work in progress: “[The literature] is based on meta-analyses and individual studies can range anywhere from 10 percent to 90 percent—so there's a huge range depending on the study, which tells you we're still figuring this out.”
Unique Challenges for AuDHDers
People with autism and ADHD have to deal with a lot, because they’re usually contending with the differences and the overlaps that come with both diagnoses. In short, says Dr. Whaling, “It’s exhausting! It’s like being two different people trying to live in the same body.”
People with autism may “crave routine and sameness for regulation,” but their “ADHD lacks the executive functioning skills and abilities to actually carry that forward consistently,” explains Dr. Whaling. And even if you have the skills and abilities to maintain routines, “if you do it for too long, the boredom and need for novelty makes you absolutely crazy,” she continues. “So you’re stuck wanting predictability but also needing stimulation.”
Those who are AuDHD must also grapple with their hypersensitivity to certain sensory input (autism side), while at the same time, they’re seeking more stimulation (ADHD side). “So you're simultaneously overwhelmed and understimulated,” illustrates Dr. Whaling, “which is just a recipe for constant discomfort.”
Emotional dysregulation is also a unique challenge for people who are AuDHD, because, says Dr. Whaling, “you're dealing with autistic meltdowns and ADHD emotional storms.” These combined reactions can be intense, especially considering they’re “often triggered by different things or the same things in different ways.”
Strengths of Being AuDHD
Being AuDHD can certainly take a massive toll on your physical and mental health. At the same time, says Dr. Whaling, those who are AuDHD have enormous potential: “AuDHD is like having a superpower when it works in your favor.”
She highlights the moments when one’s ADHD hyperfocus aligns with their autistic special interests, as being when you can be “unstoppable.” As in, “scary-good levels of expertise and productivity.”
Since ADHD provides “out-of-the-box, divergent thinking,” and autism “brings systematic analysis and pattern recognition,” having both conditions allows people to “come up with really innovative solutions that other people might not see, then actually think through the details in ways that make them workable,” observes Dr. Whaling.
Plus, those who are AuDHD have certain lived experiences that are likely unknown to neurotypical people. “AuDHD people have an incredible sense of justice and fairness,” says Dr. Whaling, “plus really intense empathy for marginalized groups—probably because they know what it's like to be misunderstood from multiple angles.” The ADHD emotional intensity, combined with autistic pattern recognition, “can make you really good at seeing systemic issues and caring deeply about fixing them.”
Finally, people who are AuDHD are more “refreshingly authentic and genuine,” says Dr. Whaling. This is because both conditions can make masking a challenge, and “pretending to be neurotypical is just too exhausting and complicated when you're managing two different neurotypes.”

How Autism and ADHD Are Diagnosed
Autism
Autism “Autism Spectrum Disorder (ASD) is a behavioral/clinical diagnosis made by a licensed professional through developmental history, behavioral observation" and standardized assessment instruments, says Debra Kissen, Ph.D, a licensed clinical psychologist and the CEO and founder of Light on Anxiety CBT Treatment Centers.
To diagnose ASD, Dr. Kissen explains, several DSM-5 criteria are necessary. These include:
- Social communication/interaction differences (all three required):
- Deficits in social-emotional reciprocity
- Deficits in nonverbal communicative behaviors
- Difficulties developing, maintaining, or understanding relationships
- Restricted/repetitive patterns (two or more required):
- Stereotyped/repetitive movements or speech
- Insistence on sameness or inflexible routines
- Highly restricted, fixated interests
- Hyper-/hyporeactivity to sensory input
- Symptoms present early in development (though may be masked until later).
- Clinically significant impairment.
- Not better explained by intellectual disability alone.
Some common assessment instruments used by professionals during an autism assessment for adults can be (but are not limited to):
- ADOS-2 (Autism Diagnostic Observation Schedule, Second Edition): A standardized, semi-structured assessment used to observe and evaluate social communication, interaction, and restricted or repetitive behaviors associated with autism.
- MIGDAS-2 (Monteiro Interview Guidelines for Diagnosing the Autism Spectrum, Second Edition): A qualitative, interview-based assessment that guides clinicians in gathering rich, descriptive information about an individual’s social communication, sensory processing, and behavior across settings.
- SRS-2 (Social Responsiveness Scale, Second Edition): A standardized rating scale completed by the individual or others that measures social awareness, cognition, communication, motivation, and interests or behaviors.
- SCQ-Lifetime (Social Communication Questionnaire – Lifetime Form): A caregiver-report screening tool designed to evaluate lifetime patterns of communication and social functioning that may indicate the presence of autism spectrum disorder.
Keep in mind that these are screeners used by diagnostic professionals. If you suspect you might be autistic, there are some self-assessment tools available, including the Autism Spectrum Quotient (AQ) and the RAADS-R. While neither of these tools can offer an official ASD diagnosis, they may help you decide if a formal evaluation is necessary.
There are also several challenges when it comes to diagnosing autism in women and other marginalized groups. Since women and people assigned female at birth are more likely to engage in masking, this, says Dr. Kissen, “can delay or complicate an accurate diagnosis.”
Other potential reasons for undiagnosed autism, delays, or complications in an accurate diagnosis, says Dr. Kissen, include cultural/racial bias toward BIPOC groups, as well as “symptom overlap with ADHD/anxiety.”
ADHD
“ADHD is diagnosed clinically through multi-informant reports, developmental history, and impairment across settings,” explains Dr. Kissen.
As with autism, ADHD is diagnosed using several necessary criteria from the DSM-5. The following nine inattention traits and nine hyperactivity-impulsivity traits are reviewed first:
- Often fails to give close attention to details or makes careless mistakes in schoolwork, at work, or with other activities.
- Often has trouble holding attention on tasks or play activities.
- Often does not seem to listen when spoken to directly.
- Often does not follow through on instructions and fails to finish schoolwork, chores, or workplace duties (e.g., loses focus, sidetracked).
- Often has trouble organizing tasks and activities.
- Often avoids, dislikes, or is reluctant to complete tasks that require mental effort over a long period of time (such as schoolwork or homework).
- Often loses things necessary for tasks and activities (e.g. school materials, pencils, books, tools, wallets, keys, paperwork, eyeglasses, mobile telephones).
- Is often easily distracted.
- Is often forgetful in daily activities.
Hyperactivity-Impulsivity traits:
- Often fidgets with or taps hands or feet, or squirms in seat.
- Often leaves seat in situations when remaining seated is expected.
- Often feels restless.
- Often unable to take part in leisure activities quietly.
- Is often “on the go,” acting as if “driven by a motor.”
- Often talks excessively.
- Often blurts out an answer before a question has been completed.
- Often has trouble waiting their turn.
- Often interrupts or intrudes on others (e.g., butts into conversations or games).
Adults (17 and older) must present with five or more of the above inattention and/or hyperactivity-impulsivity traits. In addition, several of these characteristics must have been present before age 12, and at least two traits must be present across two or more settings, such as home, school, or work. Finally, “clear functional impairment is not better explained by another condition,” says Dr. Kissen.
The common screeners used to diagnose ADHD in adults are:
Some common assessment instruments used by professionals to assess ADHD for adults can be (but are not limited to):
- DIVA-5: DIVA-5 stands for the Diagnostic Interview for ADHD in Adults – Fifth Edition. It is a structured clinical interview based on DSM-5 criteria that provides a detailed assessment of both childhood and adult ADHD symptoms across multiple life domains.
Common screeners might include:
- ASRS: ASRS stands for the ADHD Self-Report Scale. It is an 18-item self-report questionnaire developed by the World Health Organization to screen for symptoms of attention-deficit/hyperactivity disorder in adults. It assesses the frequency of inattentive and hyperactive-impulsive behaviors associated with ADHD.
- BAARS-IV: BAARS-IV stands for the Barkley Adult Attention-Deficit/Hyperactivity Disorder Rating Scale – Fourth Edition. It is a standardized rating scale designed to assess current and childhood ADHD symptoms, as well as associated functional impairments, based on DSM-5 diagnostic criteria.
As with autism, there are several challenges when it comes to diagnosing ADHD in women and people in other marginalized communities. Dr. Kissen mentions that underdiagnosis occurs with women due to their “less overt hyperactivity.” Cases of undiagnosed ADHD in women can also be due to racial/ethnic disparities, and overcompensation and masking in high achievers. Dr. Kissen also highlights a similar overlap with autism diagnoses and ADHD diagnoses: Just as an autism diagnosis can be affected by ADHD, “comorbidity with anxiety, depression, and/or autism” can complicate an ADHD assessment.
Prosper Health does not currently provide formal diagnoses for Attention Deficit Hyperactivity Disorder (ADHD). However, Prosper does provide neurodivergent-affirming therapy for those diagnosed with ADHD or who suspect ADHD (and other forms of neurodivergence).
Treatment and Support Options
One of the areas where autism and ADHD differ is in the treatment and support options for each diagnosis, specifically when it comes to therapy and medication. However, one similarity is the necessity of neurodiversity-affirming care in both cases.
Autism
- Therapy: Options for autistic adults with high support needs might include speech and occupational therapy (OT), augmentative and alternative communication (AAC), and social learning (a direct focus on enhancing one’s social skills). For lower support needs autistic adults Dr. Kissen recommends adapted cognitive behavioral therapy (CBT) for anxiety. Dialectical Behavior Therapy (DBT), and mindfulness based approaches like acceptance and commitment therapy (ACT) are also effective.
- Medication: Although autism patients can be prescribed certain medications for co-occurring diagnoses such as, per Dr. Kissen, irritability (atypical antipsychotics), ADHD (stimulants), and anxiety (SSRIs), it’s important to remember that medication is not used to treat autism itself.
- Neurodiversity-affirming care: Finding the right kind of support system is paramount for anyone with an autism diagnosis. Whether it’s your clinicians or community, neurodiversity-affirming care “prioritizes autonomy, quality of life, and authentic communication over ‘masking,’” says Dr. Kissen.
ADHD
- Therapy: Dr. Kissen recommends CBT for adults with ADHD. The goal of this type of therapy is to lessen the inattention and impulsivity common with ADHD patients. Therapists can work with you on developing time management and scheduling skills, organizational habits, and coping strategies for completing tasks in a timely fashion. Another therapy Dr. Kissen recommends for adults with ADHD is executive functioning coaching. Executive functioning is an umbrella term for everyday skills like working memory, cognitive flexibility, and inhibition control. All help you manage everyday tasks like making plans, solving problems, and adapting to new situations.
- Medication: Stimulants are the most common type of medication prescribed for people with ADHD. These medications work by increasing levels of certain chemicals (neurotransmitters) in the brain that are integral for paying attention, thinking, and remaining motivated.
- Neurodiversity-affirming care: As with autism, neurodiversity-affirming care is essential to leading a full and fruitful life with ADHD. This type of support system, according to Dr. Kissen, “frames ADHD as a difference, not a failing. [Neurodiversity-affirming care also] builds supports around strengths and accommodations.”
How Prosper Health Can Help
If this article has your wheels turning about your own diagnosis, or has you thinking you might want to look into getting diagnosed for autism, Prosper Health can help.
- Diagnosis: Prosper Health offers guidance through every step of your diagnostic journey via telehealth autism assessments from clinicians whose specialty is working with autistic adults. And yes, many forms of insurance are accepted.
- Therapy: Prosper Health also provides ongoing, individualized support for autistic people and AuDHDers through neurodiversity-affirming therapy. The clinicians and therapists at Prosper Health are experts in supporting neurodivergent adults. While working with Prosper Health you’ll be matched with a therapist who will help you meet your goals and discovering ways to thrive as an autistic person.
Conclusion
The more we understand about the differences and overlaps between autism and ADHD, the closer we can get to developing the kind of holistic support systems that AuDHD people need. In full transparency, this goal is still a work in progress: “We’re still figuring it out,” says Dr. Whaling of parsing the differences and similarities between autism and ADHD. “So if you're feeling confused or like the information keeps changing, that's because it literally is.”
However, since the research on people who are AuDHD is evolving, Dr. Whaling points out that “a lot of folks got misdiagnosed with anxiety, depression, bipolar disorder, personality disorders, or just told they were ‘difficult’ or ‘sensitive’ when really they were autistic or had ADHD or both.”
Above all, whether you’re ADHD, autistic, AuDHD, or a neurotypical person with quirks, remember that “you're a whole, complete, worthy human being deserving of understanding and support,” assures Dr. Whaling.
Frequently Asked Questions (FAQs)
What is the difference between ADHD and autism?
While both autism (ASD) and ADHD are neurodevelopmental conditions with overlapping traits, their key differences lie in their core diagnostic criteria and the underlying reasons for similar behaviors.
How do I know if I have ADHD or autism?
There are specific criteria for diagnosing either ADHD and/or autism through a variety of diagnostic screeners. A qualified clinical provider can conduct these evaluations. Self-assessment autism questionnaires, such as the Autism Quotient (AQ) and the RAADS-R, while helpful, cannot provide official diagnoses.
Can autism look like ADHD?
Yes, autism can look like ADHD due to overlapping traits, particularly in areas like social communication, routines, intense interests, and sensory differences. However, the underlying reasons for these outwardly similar behaviors often differ between the two conditions.
Is hyperfixation a trait of ADHD?
Yes, hyperfocus (a form of hyperfixation) can be a trait of ADHD. While an autistic person's intense interests are often a core part of their identity, for people with ADHD, a hyper-focused interest in something has the potential to be more fleeting.
Is hyperfixation a trait of autism?
Yes, intense, highly restricted, or fixated interests, which can be seen as a form of hyperfixation, are a diagnostic criterion and common trait of autism.
Are autism and ADHD related?
Yes, autism and ADHD are related. They are both neurodevelopmental conditions with overlapping traits but distinct underlying causes.
Sources
https://www.prosperhealth.io/blog/what-is-audhd
https://www.prosperhealth.io/blog/autism-and-stimming
https://health.clevelandclinic.org/adhd-vs-autism
https://pubmed.ncbi.nlm.nih.gov/35295773/
https://autism.org/what-is-autism/
https://www.cdc.gov/autism/about/index.html
https://my.clevelandclinic.org/health/articles/autism
https://my.clevelandclinic.org/health/diseases/4784-attention-deficithyperactivity-disorder-adhd
https://www.psychiatry.org/patients-families/adhd/adhd-in-adults
https://my.clevelandclinic.org/health/diseases/15253-inattentive-adhd
https://www.research.chop.edu/car-autism-roadmap/social-responsiveness-scale-second-edition-srs-2
https://pmc.ncbi.nlm.nih.gov/articles/PMC10060524/
http://cdc.gov/adhd/diagnosis/index.html
https://pmc.ncbi.nlm.nih.gov/articles/PMC6585602/
https://novopsych.com/assessments/diagnosis/adult-adhd-self-report-scale-asrs/
https://my.clevelandclinic.org/health/treatments/24692-antipsychotic-medications
https://my.clevelandclinic.org/health/treatments/11766-adhd-medication
https://my.clevelandclinic.org/health/treatments/24795-ssri
https://my.clevelandclinic.org/health/articles/executive-function
Related Posts
.webp)
Autism and Co-Occurring Conditions: A Guide
Autism is known to co-occur with several health conditions—but what does this mean? What other diagnoses are most prevalent among autistic individuals, and does an autism diagnosis inform treatment of co-occurring conditions?
.webp)





